Advances in medical technology have transformed human lives in many ways, allowing us to live far longer and to cure numerous conditions. But not all of us – especially those who are laymen – are certain about whether the shiny new equipment or the latest innovations we read about are truly more effective or if they only show hypothetical benefits. The Chinese University of Hong Kong (CUHK)’s medical scientists are keen to debunk this myth to help people make informed decisions, enabling both clinics and patients to better allocate precious resources, focusing on changes that are genuinely effective.
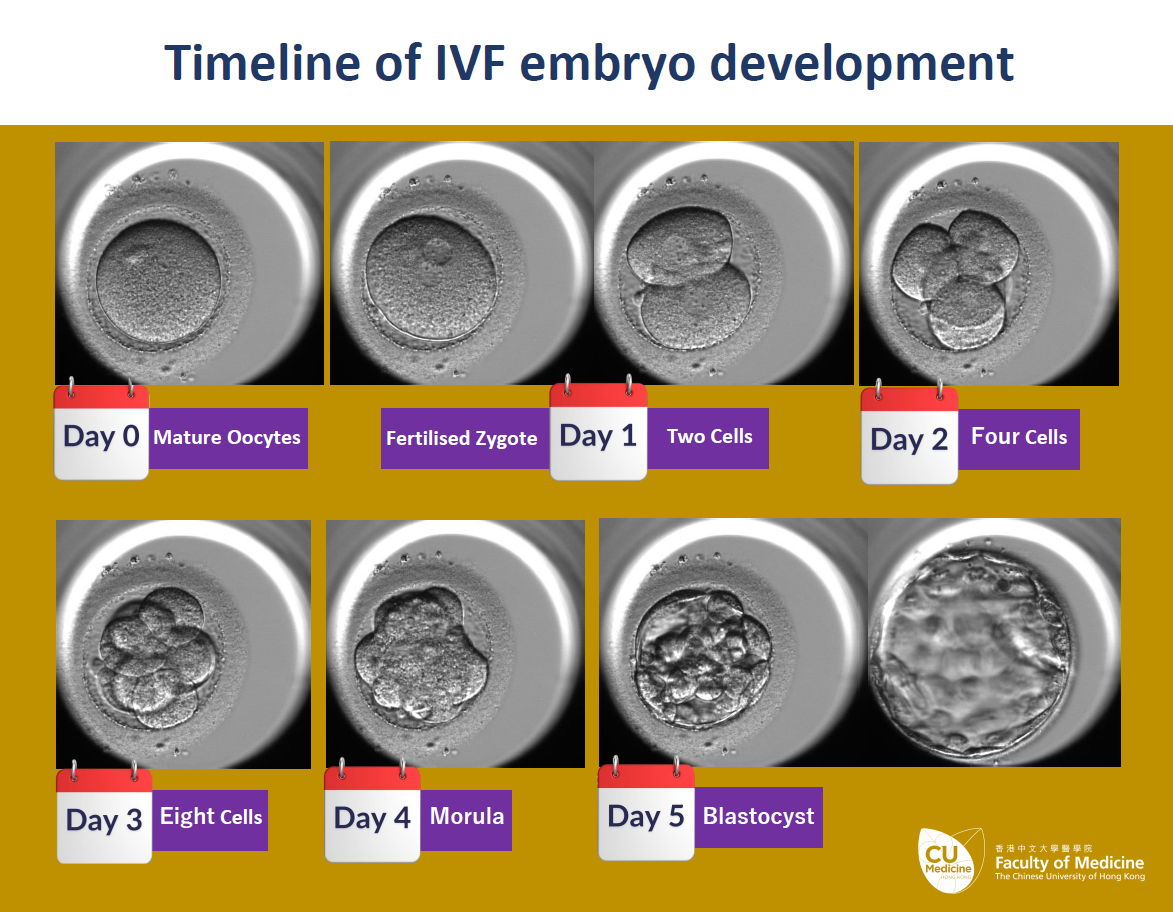
One such innovative technology that CUHK scientists have been investigating is the time-lapse imaging (TLI) systems that are often used while incubating embryos during in vitro fertilisation (IVF). Infertility affects about one in six people trying to conceive, and IVF is one of the most effective ways of helping them. It involves extracting eggs and sperm, combining them in a petri dish, and then incubating the resulting embryo in a laboratory, typically for about five days, before injecting it into the uterus of the prospective mother. Naturally, there’s nothing more important to anyone than the health of their potential child, and so everyone is keen for the systems used to protect the fertilised embryos to be as safe, effective and efficient as possible.
What really works?
For about 15 years, TLI systems have been a popular option in developed countries to monitor most embryos using cameras; more than 90% of IVF labs in Hong Kong, for example, are equipped with the technology. Fair enough, you might think: not only do they mean that embryos can be monitored continuously, as opposed to the conventional method, where an embryologist takes a look, typically once a day, but they also reduce the need to move the embryos in and out of incubators in order to get a good look at them – something that you’d think would necessarily help their chances of flourishing.
However, no previous study had rigorously tested whether it is really true. Moreover, IVF treatment involving TLI typically incurs an additional cost of about 5% cost due to the expensive equipment used. That’s where CUHK has stepped in.
The Assisted Reproductive Medicine Unit in the Department of Obstetrics and Gynaecology within CUHK’s Faculty of Medicine (CU Medicine), together with its partner, the Women’s Health Research Unit at Queen Mary University of London, has conducted the largest international trial regarding TLI to see which methods of embryo management are most effective: it involved 1,525 patients, two-thirds of them in the UK and the other third in Hong Kong.
“We encourage randomised controlled trial (RCT) studies to support evidence-based medicine refuting hypothetical benefits without proven clinical outcomes,” says Dr Jacqueline Chung Pui-wah, Director of the Reproductive Medicine Unit in the Department of Obstetrics and Gynaecology at CU Medicine. “However, it is very challenging and takes a tremendous effort to conduct a multi-centre RCT with a large cohort size and follow up to the live birth,” hence no one had managed to do so.
The trial divided the participants into three groups: one set had embryos assessed by a fully automated system with TLI and automatic selection based on the morphological embryo scoring provided by the system; a second were monitored by TLI, but with a human embryologist performing the embryo assessment; while a third received conventional treatment, with embryologist grading but no use of TLI. The results weren’t what you might instinctively expect: there were no major differences among the three groups when it comes to pregnancies and live births, although TLI still has the advantage of seamless monitoring. The landmark findings have been published in The Lancet.
As a result, the researchers recommend that IVF clinics focus on equipment and methods with proven positive impact, such as better injection systems, media, preparations and so on; and patients seeking IVF treatment are more vigilant about the fees they pay for embryo culturing: paying more does not necessarily lead to better results.

Don’t abandon TLI
That doesn’t mean TLI systems aren’t useful, however; they could still enjoy several major advantages over conventional culturing systems. This particular experiment, says Lab director Assistant Professor David Chan, “reflects that TLI does not work in this dimension. However, the usefulness of TLI has not been fully scrutinised holistically in this study, such as the power to de-select by embryo features, to exclude things like abnormal development from the embryo transfer. It only showed the clinical live birth rate from a patient’s perspective.”
Following on from their landmark findings, the team aren’t resting on their laurels. Again in partnership with Queen Mary University of London, the CUHK researchers are currently conducting the world’s largest independent patient data (IPD) meta-analysis of TLI, which is scheduled to be published in autumn 2025. It will be able to provide a far more detailed picture of the systems’ effectiveness, and a more detailed information about outcomes in various places. Armed with that information, IVF units should be able to nurture more bouncing babies safely into the world, providing embryos with the best possible care – and making a million parents’ dearest dreams come true.